The Crucial Role of Medical Billing Software: Enhance Healthcare Revenue
The Crucial Role of Medical Billing Software: Enhance Healthcare Revenue
January 8, 2024
In today’s complex and competitive healthcare landscape, maximizing revenue is not just about delivering excellent care. Medical practices face mounting administrative burdens, convoluted coding regulations, and ever-tightening reimbursement margins. This is where medical billing software emerges as a crucial ally, transforming the revenue cycle from a cumbersome chore into a streamlined engine for financial growth.
Mammoth patient data and multiple billing needs across departments can create pressure on billing systems. Hence, it becomes important to regulate the billing mechanism with competent medical billing software that can help you save time, cut costs, and minimize potential errors in billing.
While those are a few advantages that an integrated billing system can offer your medical center, find out more on how you can use software to improve healthcare revenue.
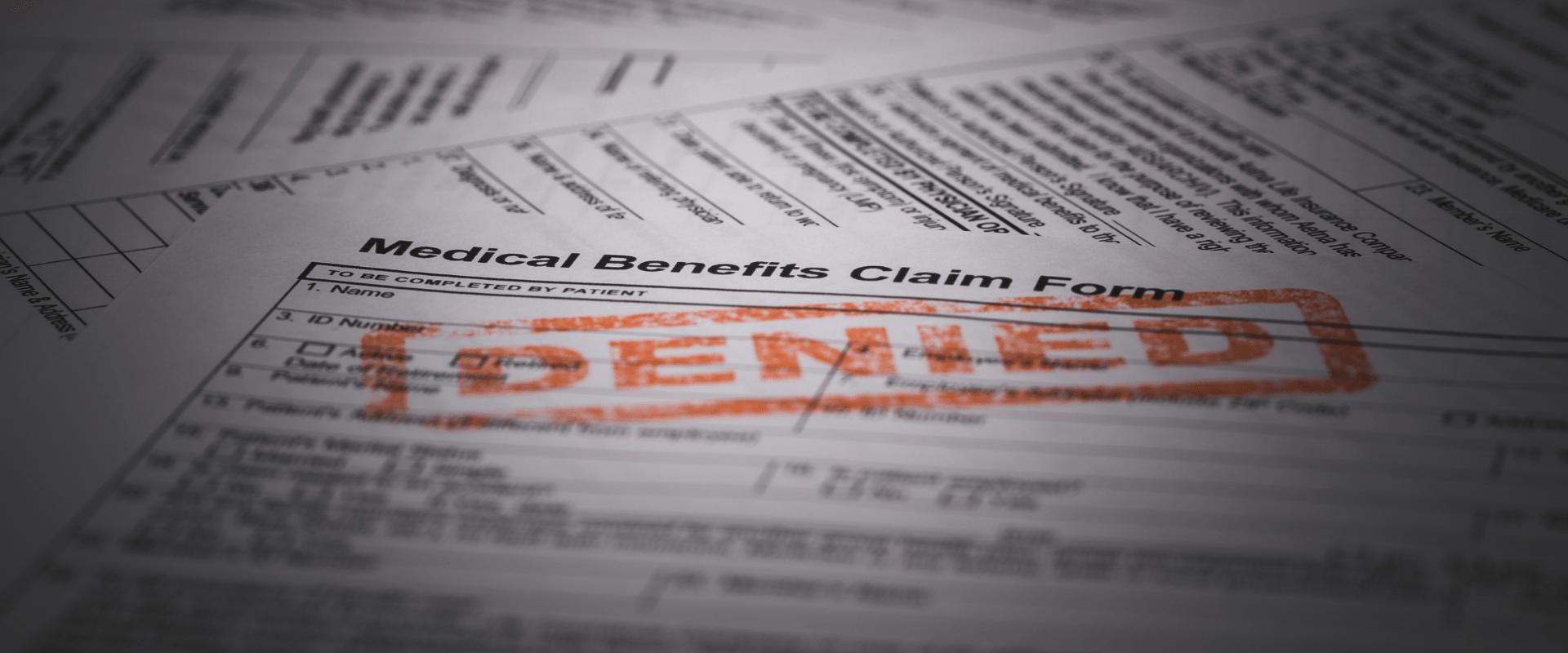
Traditional Systems and Their Challenges:
For decades, healthcare relied on a patchwork of traditional systems to manage its complex workflows. However, these time-worn tools are increasingly proving inadequate, riddled with pitfalls that threaten efficiency, accuracy, and trust. Let’s delve into some of the most pressing challenges plaguing these legacy systems:
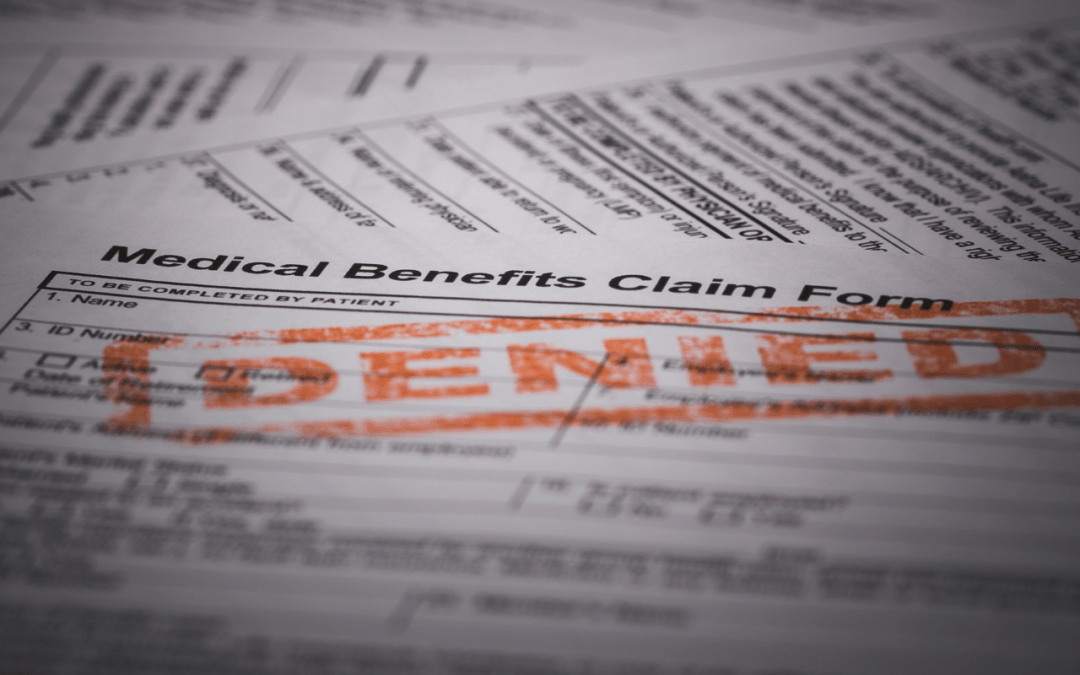
- Coding Errors: Manual coding errors, like upcoding or downcoding, wreak havoc on claims, delaying reimbursements and draining resources.
- Inaccurate Patient Data: Mountains of patient information lead to misrecording and duplicate billing, tarnishing patient trust and impacting bottom lines.
- Denials: Missing documentation and insurance verification complexities cause claim denials and lost revenue, adding another layer of frustration.
OmniMD’s RCM software is designed to address these issues:
- Automate Claim Processing: Claims are submitted and tracked electronically, reducing processing time by 30% and accelerating reimbursements.
- Minimize Errors: OmniMD’s automation ensures 100% coding compliance and minimizes errors, leaving you with less than 5% denial rates.
- Boost Operational Efficiency: By automating repetitive tasks and streamlining workflows, OmniMD frees up your staff time which can be utilized on high-value activities like patient consultations, new patient acquisition, and insurance follow-up, which can directly boost your revenue potential.
- Improve Cash Flow: Automated claims processing accelerates reimbursements by 30%, putting 10% more cash in your pocket every month.
- Enhance Patient Satisfaction: Online bill pay, appointment reminders, and secure portals offer a convenient and transparent patient experience.
Medical Billing Software
A medical billing software system is an electronic accounting application that can be used by healthcare centers to streamline patient billing data, process invoices, and regulate payment services. This automated system can process both physical billing data and e-data to help you keep account of how much your customers owe you for the products and services delivered to them by your medical center.
While standard solutions often focus on automating tasks like claim submission, OmniMD delves deeper, offering a comprehensive suite of features designed to optimize every aspect of the revenue cycle:
Front-Office Automation
Front-office automation is designed to enhance operational efficiency by optimizing various tasks such as scheduling, eligibility checks, and online payments. This comprehensive solution incorporates automated reminders and secure patient portals to facilitate a seamless experience.
OmniMD stands out for its remarkable acceleration in documentation times, achieving a notable reduction of 180 seconds for new patients and 45-60 seconds for established patients, surpassing industry averages. This not only streamlines administrative processes but also ensures a swift and efficient workflow for healthcare providers.
Back-Office Efficiency
This is precisely where advanced features come into play. OmniMD offers a sophisticated solution geared towards eliminating errors and reducing delays through the implementation of cutting-edge claim scrubbing, denial management, and the generation of insightful billing reports.
What sets OmniMD apart is its real-time monitoring and analysis. The utilization of dynamic dashboards ensures that administrators have access to actionable insights promptly. This proactive approach enables healthcare providers to identify and address potential issues before they can have a detrimental impact on reimbursement processes.
OmniMD not only streamlines back-office operations but also empowers organizations to maintain a high level of accuracy, thereby fostering a more efficient and resilient healthcare billing system.
Maximizing Recoveries
OmniMD’s ARQ Manager revolutionizes revenue recovery in healthcare by automating tasks with features like customizable letters and paperless document storage. This advanced tool streamlines collections, freeing up staff to focus on essential patient care, and making the process more efficient and patient-centric.
OmniMD automates data capture, ensuring reliable information and reducing claim rejections by less than 5%.
Billing Analytics
Billing analytics becomes a powerful ally for healthcare practices through OmniMD’s advanced features. The platform offers configurable billing profiles and user productivity tracking, providing valuable insights into practice performance. OmniMD’s intuitive dashboards facilitate data-driven decision-making, enabling practices to maximize revenue and optimize operational efficiency.
How OmniMD Can Make a Difference
Apart from its feature-rich platform, OmniMD stands out for its commitment to your success:
- Scalability and Affordability: OmniMD caters to practices of all sizes with flexible pricing plans that align with individual needs.
- User-Friendly Technology: The intuitive interface ensures seamless adoption and minimizes training time for staff.
- Exceptional Support: OmniMD offers free onboarding, phone and email support, and online training, ensuring practices have the resources to thrive.
- Proven Track Record: With over 20 years of experience, OmniMD boasts a 99% customer retention rate and 99.95% uptime, testifying to its reliability and effectiveness.
Bottom Line
Investing in medical billing software isn’t just a cost; it’s an investment in your practice’s future. Imagine a world where paperwork doesn’t pile up, claims get processed at lightning speed, and your bottom line sings a happy tune. With OmniMD, that world is within reach.
Don’t let outdated systems hold you back. Embrace the revolution, unlock your revenue potential, and watch your healthcare practice thrive.